SPECIAL REPORT: Unsung heroes keep hospitals running smoothly during the pandemic
Throughout 2020, much news has focused on the doctors and nurses fighting on the front lines of the battle against COVID-19. But behind the scenes, there is an entire echelon of support staff.
Throughout 2020, much news has focused on the doctors and nurses fighting on the front lines of the battle against COVID-19. But behind the scenes, there is an entire echelon of support staff making sure each patient, employee, and guest is protected against the spread of the deadly virus.
“When the pandemic hit, we put a number of our projects into a suspended status that were underway or in the planning process at the time, and really focused on what our immediate needs were as a system,” says Mark Hisey, Vice President of Planning, Design, and Construction for Parkview Health.
Hisey leads a team of 14 people who work throughout all of Parkview’s facilities, developing the long-term plans for different facilities and campuses, and overseeing design, major construction projects, and wayfinding/signage. The team includes interior designers, licensed architects, construction managers, and even a clinical specialist who is a masters-level registered nurse.
He says, “A big part of our process was identifying and implementing a strategy for how we can keep our coworkers and patients safe through this pandemic through negative-pressure-room development.”
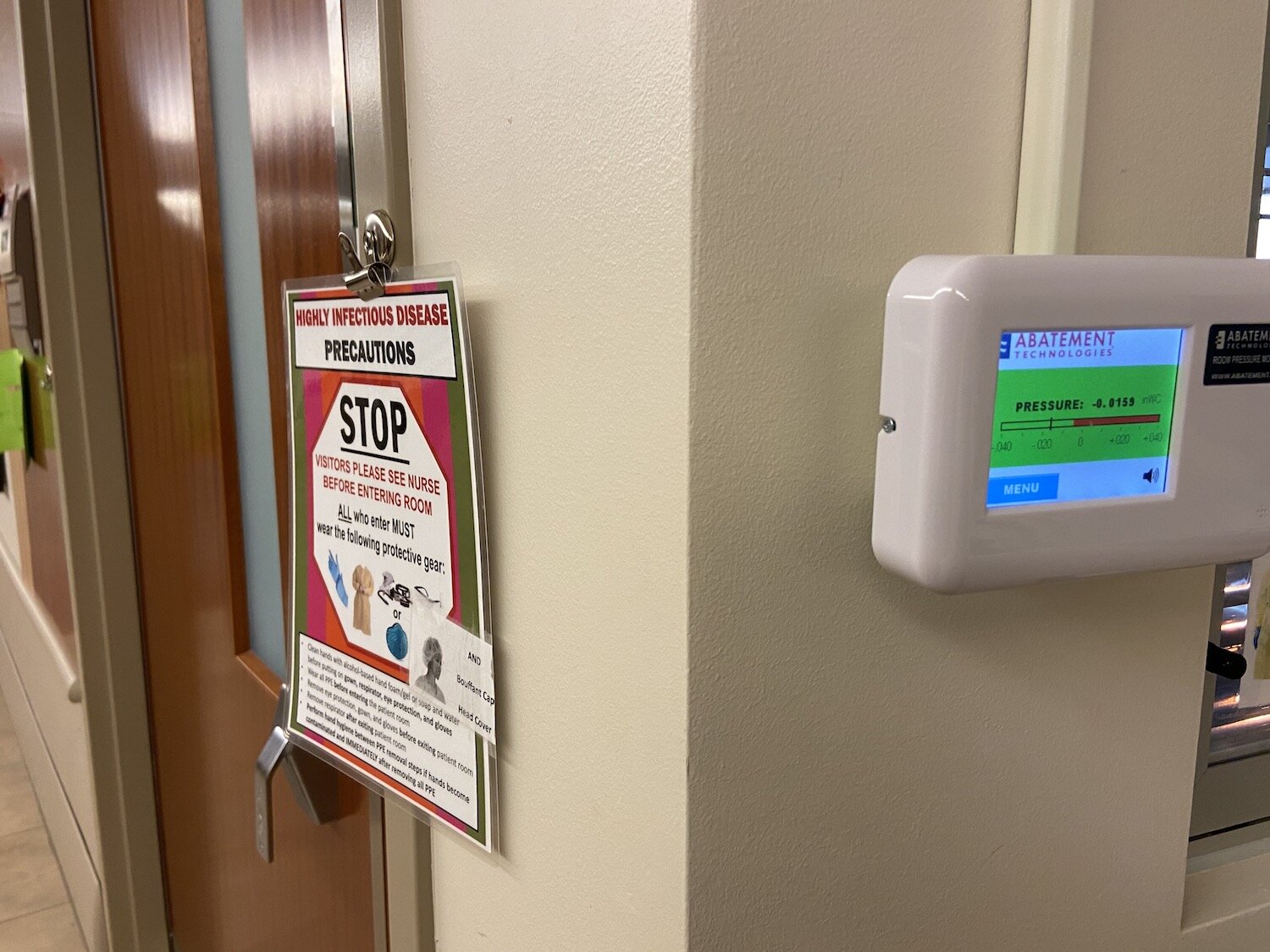
A negative pressure room—also known as an airborne-isolation room or airborne-infection-isolation room—is a room where the supply and exhaust of air creates a condition so that whatever’s in the air within that area cannot escape into other parts of the hospital.
“It basically takes bacteria, viruses, germs, everything else that’s in the air of that room, and exhausts it directly outside,” Hisey says. “It creates a controlled vacuum within that room, so that the air from that room doesn’t seep over into the adjacent patient room or out into the hallway where other people could be infected.”
Some parts of the hospital contain common ductwork that may connect 10 rooms, allowing all 10 of those rooms now to become negative-pressure. Hisey’s staff have converted more than 200 inpatient rooms and exam rooms within Parkview’s emergency departments to negative pressure.

Keeping the campuses clean is the role of the Environmental Services (EVS) crew. Although they’ve always had strict policies regarding sanitation and germ containment, the pandemic has forced them to up their game.
The new process involves spraying the room with Concept 256N disinfectant and then running a Tru-D UV light for 10 to 30 minutes, depending on the room. Employees protect themselves by wearing personal protection equipment (PPE) that includes powered air-purifying respirators (PAPRs) that wrap around the head and cover the mouth and nose, filtering the air with a battery-powered machine.
To communicate with each other, they use iPads loaded with the Epic Rover app to signal when a patient’s room is ready to be cleaned.
“When there’s a discharge of a room in the system, we receive a notification,” says Latisha Lattimore, EVS Supervisor for Parkview Regional Medical Center. “We have secure chat, so we message back and forth. It’s a great way of communicating and keeping the patient flow going.”

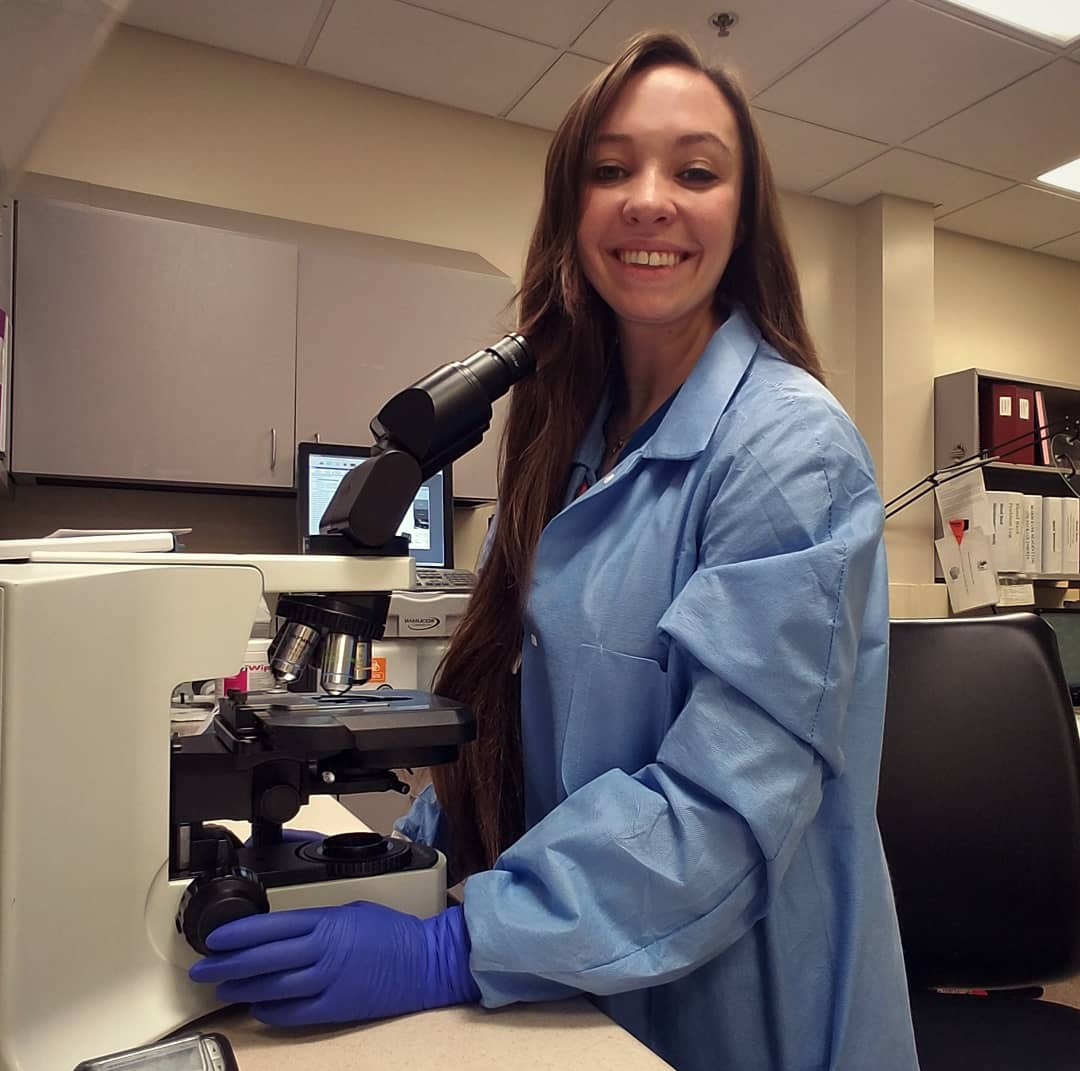
Having clean campuses protects the patients, guests, and other employees, like Megan Ledford, a Medical Laboratory Scientist at Parkview Huntington Hospital. Her daily routine includes chemistry work, hematology, urinalysis, and microscopic examinations. The COVID-19 pandemic has increased her already heavy workload of cancer, urinary tract infections, respiratory viruses, strep throat, and flu that she has to test for.
“Obviously, the volume that we’re dealing with right now is crazy,” she says. “There are so many people, especially with the winter surge that we’re having. Anytime someone comes in with any type of symptom of fever or runny nose, we run the whole gamut of testing for those patients, which is quite a bit.”
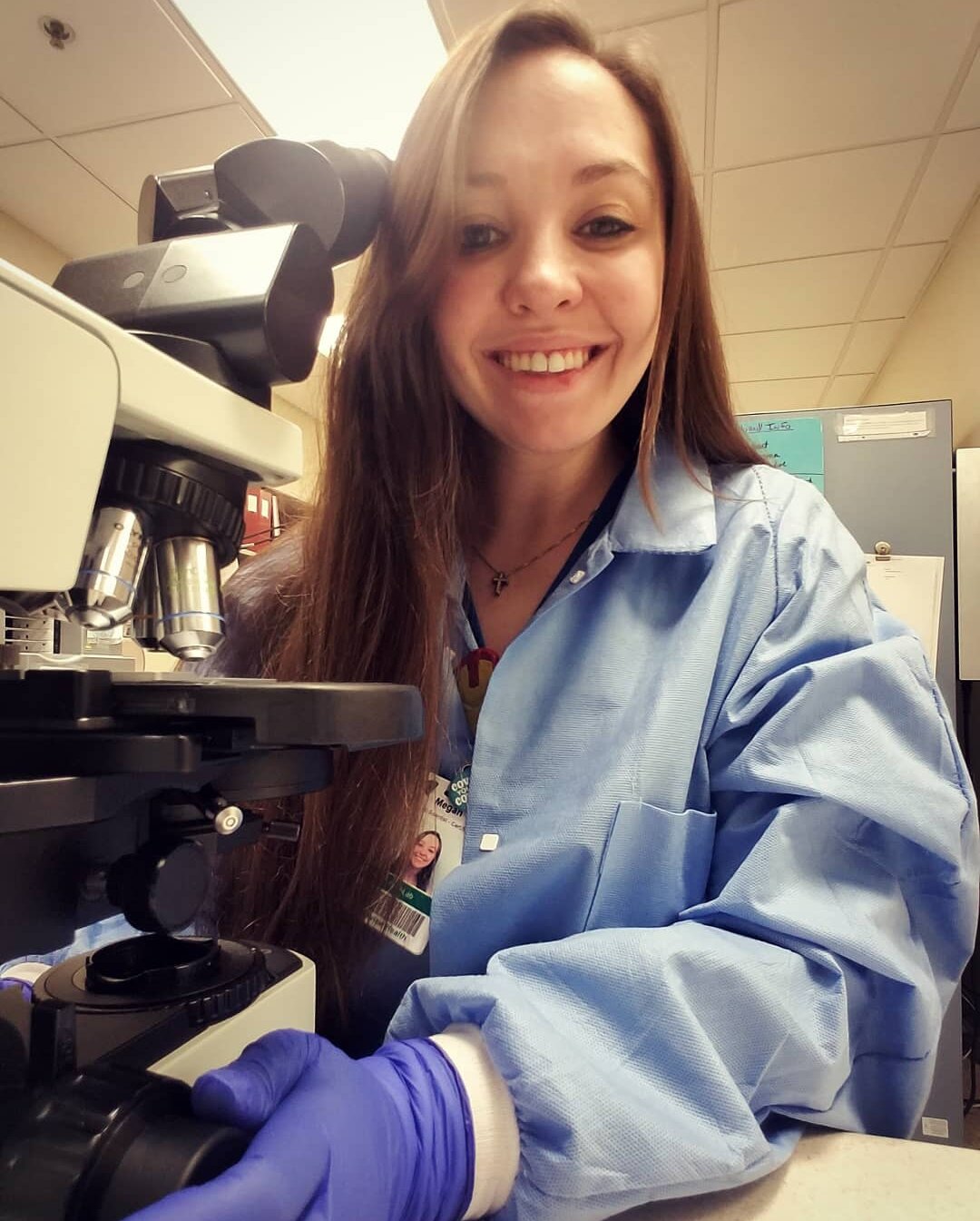
Policies and procedures change all the time. That’s nothing new in the science community. But when a pandemic hits during flu season, the struggle turns up a notch, forcing staff to deal with stock shortages, new testing requirements, and a high volume of specimens that need to be processed quickly, accurately, and efficiently.
Ledford says about 10 percent of her workload is devoted to COVID-19 alone. Much of it has to do with implementing new tests and treatment options, like antibody testing and convalescent plasma.
“We’ve been giving out tons of that (convalescent plasma), and it’s been really great,” she says. “People get tested for the antibodies, and if they have them, they can get plasma drawn. The antibodies that are in your plasma can be transfused to another patient.”
“We need everybody’s help in trying to help stop the spread of COVID-19,” Hisey says. “It’s really going to take everybody’s concentration and focus to get this stopped.”
This Special Report is made possible by Parkview Health.











