SPECIAL REPORT: Taking a human-centered approach to healthcare innovation
Parkview Health is increasing access to healthcare with new technology and treatment methods that put people first.
The opioid epidemic. Rural access to regional specialists. Affordable, personalized preventative care.
These health issues are at the top of mind for medical professionals in northeast Indiana, so it’s no secret that the region’s largest healthcare provider, Parkview Health, is taking innovative measures to address them.
Parkview is often known for pushing the boundaries of innovation, boosting public health, and increasing its efficiency. But while patients and residents might assume that “innovation” means using the latest technology or making new medical discoveries, innovation in healthcare also requires a relational aspect, says Sara GiaQuinta, Vice President of Community Health for Parkview.
More than anything else, relationships need to be at the heart of an innovative approach, she explains.
“Often, when people think of innovation, they think of some never-before-tried thing, but the biggest part of success is the relationship component,” GiaQuinta says. “How do we bring that to other areas of healthcare? I don’t think that can be overlooked.”

Here are three ways Parkview Health is embracing a people-centered approach innovative strategy to boost health outcomes and quality of life across northeast Indiana.
Using a smartphone app to take on the opioid epidemic
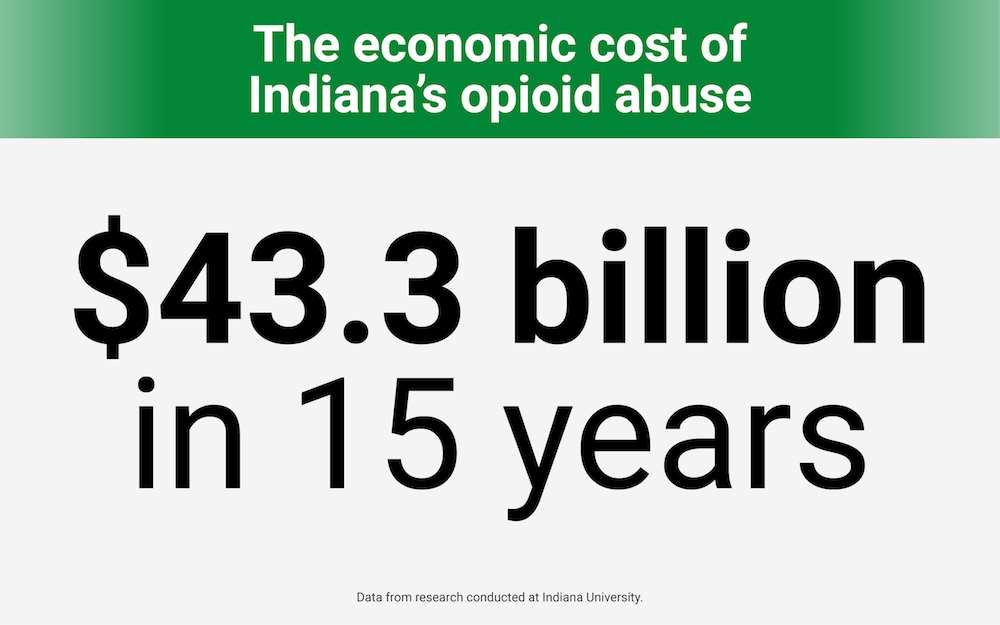
To quantify the extent and severity of the opioid problem in Indiana, the National Institute on Drug Abuse reports that the age-adjusted rate of drug overdose deaths in the state rose from 24 per 100,000 in 2016 to 29.4 per 100,000 in 2017.
On top of that, 15 years of opioid abuse in the state has cost Indiana $43.3 billion in economic losses, according to two Indiana University researchers.
“This is one of the largest public health concerns that many of us will see in our careers,” says Connie Kerrigan, Director of Outreach at Parkview Behavioral Health. “It’s like walking in a war field, trying to see how you can pull people out of battle and help them.”
Under the leadership of Kerrigan and Tammy Toscos, Research Scientist and Informatics Manager at Parkview’s Mirro Center for Research and Innovation, Parkview is developing a smartphone app that will address the needs of those negatively impacted by opioids. The American Hospital Association was so impressed by these efforts that it awarded Parkview Health with first-place honors (which included $100,000 in grant money) in its Innovation Challenge, which took place last year. Parkview prevailed over 90 other organizations that entered the Challenge.
But even though smartphone technology will ultimately enable the app, human connection is at its root, Kerrigan says. As part of the program, Parkview has hired six full-time peer recovery coaches who residents in need can connect with. When someone needs help, they can reach a peer recovery coach via the app, combining technology with human connection.
“Three teams—behavioral health, research, and innovation—came together and are collaborating around recovery coaches,” Kerrigan says. “We recognized that (opioid abuse) is a large public health crisis, and we asked ourselves: What if we had technology to support what we are doing?”
In the meantime, the app is being fine-tuned and has not yet been officially released.
“We expect to work with it for at least another year until there is a final robust design,” Toscos says.
Increasing regional access to care with “virtual” visits
Skype and FaceTime are two popular methods of virtual communication. Now, Parkview Health has adopted these types of interactions, and more, to enhance access to its care across the region.
For example, video visits, in which a patient at a community hospital can virtually connect with a specialist at a regional medical center for a consultation, have been available for three years.
“So instead of being transferred from Huntington or Wabash, video visits can connect patients and doctors remotely,” says Max Maile, Parkview’s Director of Virtual Health. “Patients can still see their doctor at a community hospital, but a specialist can be involved remotely. Digital stethoscopes can transmit heart tones over the line so an assessment can be done.”
This, says Maile, is great for patients in rural areas, because it’s often easier for their friends and family members to visit if they are at a community hospital. Plus, it empowers community hospitals to care for their patients more effectively where they are.
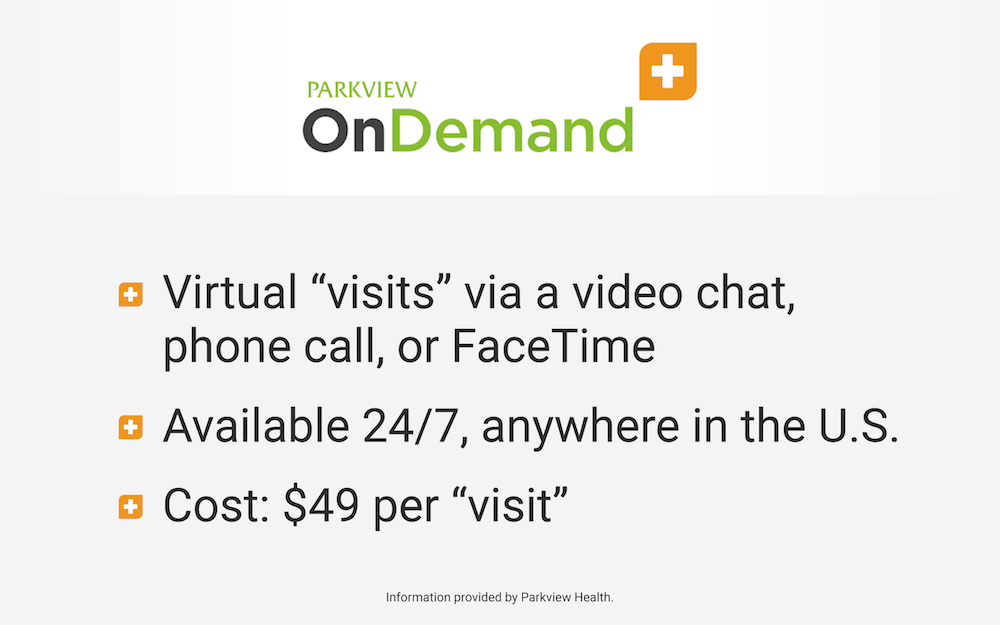
Another “virtual” innovation in healthcare is Parkview OnDemand, which offers video visits, phone calls, or FaceTime sessions with Parkview clinicians for patients anywhere in the country, 24/7. The cost for this service, which does not accept health insurance, is $49.00 per “visit.”
“It sort of operates like Uber,” says Maile, explaining that people who use this service often suffer from cold or flu symptoms, rashes, diarrhea, urinary tract infections—common issues that people would go to a walk-in clinic for.

Also, those who use this service can receive prescriptions to any pharmacy. For instance, if they are on vacation in Florida, Parkview can send their prescription to the nearest pharmacy, sans out-of-network fees.
“Parkview OnDemand is convenient when you are not feeling well or when you do not feel like going out,” Maile says. “It sends out a notification to a number of different providers, and someone will say they can go ahead and take a visit.”
Parkview also uses MyChart, a digital tool in which all charts and records are kept in the same place and are easily accessible. Patients can even request refills and schedule appointments online.
“People would just rather do online whatever they need to do instead of having to come in,” Maile says. “An example of this is the banking industry. When’s the last time you went to the bank to cash a check? Healthcare needs to be convenient—not so much about us dictating that journey. We focus on what consumers want, which is transparency and ease of access.”
Bringing nurses to the Fort Wayne Rescue Mission

A team of registered nurses from Parkview, along with a dietitian and community health worker, serve the male homeless population at a small clinic inside the Rescue Mission in Fort Wayne.
As Vice President of Community Health for Parkview, GiaQuinta views this effort as another innovation because it is meeting a need.
“A lot of men from the Rescue Center were going to the hospital via EMS or through the ER,” GiaQuinta says. “Between 2015 and 2018, that number has gone down by 50 percent.”
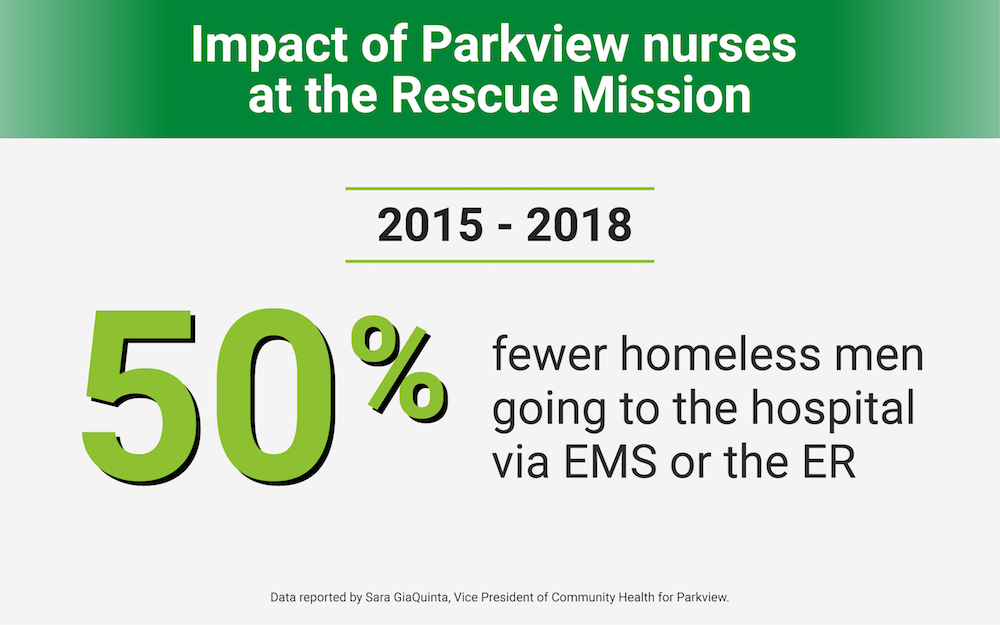
For this, she credits the presence of embedded nurses at the Rescue Center to help men with their physical health needs. They meet with Rescue Mission residents, perform a baseline physical examination, and find out if they have health insurance or a primary care physician, and then work to address whatever needs arise.
“These men need a lot—a relationship, a person they trust and can go to,” GiaQuinta says. “Our community nurses have provided wonderful stable relationships and links to healthcare.”
This Special Report was made possible by Parkview Health.










