How local organizations are using state funding to challenge the status quo around public health
“We all have to be very mindful that it's probably going to be at least 10 years until we start seeing actual changes in outcomes, such as obesity or food insecurity. As a state that took a long time to get where it got, it'll take a long time to begin to see betterment in that.”
Indiana may be known for many things: corn, the Indy 500, pork tenderloin sandwiches and other cultural touchstones. However, robust public health outcomes usually don’t rank highly on the list.
Stakeholders at the state and local levels are hoping to change that. Enter the Indiana Department of Health (IDOH)’s Health First Indiana (HFI) initiative. What the agency refers to as a “historic investment in public health” came out of 2023 legislation that was intended to re-tool the state’s approach to improving the health of Hoosiers, as reported by WFYI Indianapolis. HFI will serve nearly 96 percent of Hoosiers via $75 million in funding going to local health departments. Before this move, counties shared about $7 million from the state annually.
In a January 2024 statement, the state indicated that the money is intended to impact the local level, giving health departments resources to address critical needs, in partnership with elected officials, hospitals, clinics, and schools. Locally, Mindy Waldron serves as the administrator and deputy health commissioner of the Allen County Health Department. She oversees nearly 80 staff and all of the department’s programming. She says that while HFI funds will tackle a variety of health disparities, chronic disease is an area where there’s room for improvement in Allen County. This is among the reasons local public health officials opted to receive the nearly $9 million in funding for 2025– to take a proactive approach.
“We know that one of our larger causes of death locally and… (in) Indiana, as a whole, is heart disease, which usually is from a number of things — one of them being chronic obesity,” she says. “So when you look at root causes, one of the things that we did target some of our funding around nutrition and access to physical exercise — the prevention side of what leads to obesity, so it’s one of many things that we’re utilizing the funding for. “
Waldron says that to date, as a pass-through entity, the Allen County Health Department has awarded a little over $2 million in HFI-related grants to entities in Allen County, in 2024. This reflects about half of the total funds it received.
Each of the grantees are working to improve the population’s health and wellness, as explained in their Health First Allen County plan. Specifically, all of the HFI-funded programs reflect the county’s core public health service areas: maternal and child health, school health, trauma and injury prevention, tobacco cessation/vaping prevention, chronic disease prevention, access and linkage to care, addressing most common causes of death, and immunization. Waldron says the department elected to fund nonprofits directly instead of providing services in-house. That’s because Allen County has a strong network of nonprofits, staffed by resident domain experts working to address physical health.
For instance, HFI funds have supported hands-on programming at Fort Wayne Community Schools, nutrition classes at the YMCA, and the nonprofit Blessings in a Backpack, among others. Blessings in a Backpack is a Fort Wayne-based organization that provides food on the weekends for school-aged children who might otherwise go hungry.
According to Waldron, the HFI funding helps to increase these groups’ capacity and consequently positively touch more lives. While HFI program dollars are guaranteed through the end of 2025, her institution can only fund programs one year at a time. The grantees will need to re-apply to be considered for additional funding in 2025, she says. Applications for the 2025 grant cycle are due on or before August 30.

Among those working in the community nutrition space is Gina Dundon, who serves as the wellness coordinator at Fort Wayne Community Schools. A registered nurse by training, she’s tasked with helping the schools find programming that supports wellness activities. For instance, in partnership with the Allen County Department of Health and St. Joseph Community Health Foundation, she implemented Cooking in the Classroom.
According to the foundation’s website, the Cooking in the Classroom program reflects its work to prevent and treat chronic disease through nutrition education and access to healthy foods. They also partner with Parkview Health to provide a program called Our HEALing Kitchen, which is focused on nutrition education.
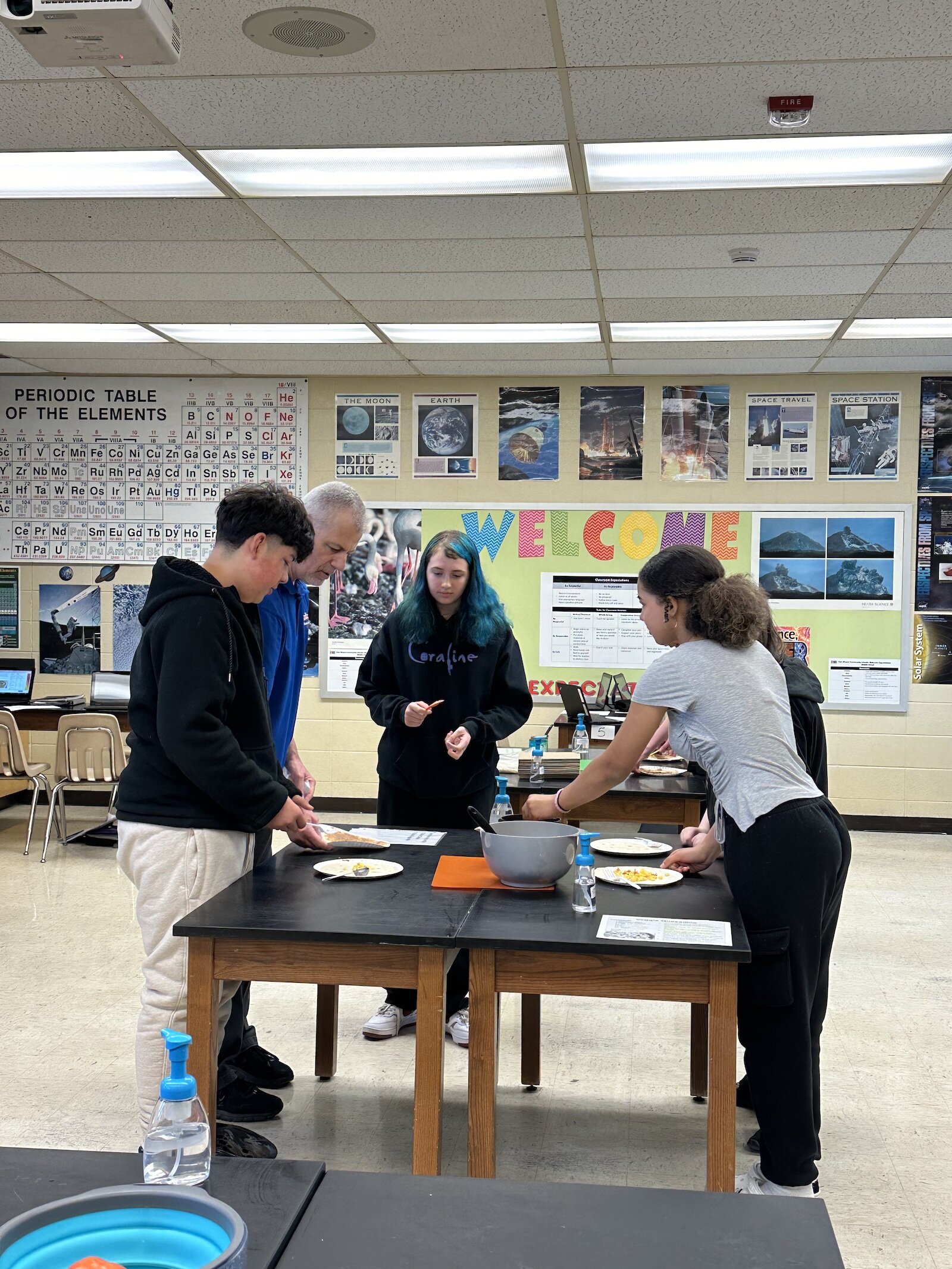
To date, Dundon says Cooking in the Classroom has engaged about 4,200 seventh-grade students across the district in cooking lessons and nutrition activities. While the volume is impressive, the net impact can be challenging to quantify because the students are asked to self-evaluate. The reality is that survey bias can skew the results because some don’t want to reveal a lack of knowledge out of a perceived fear of stigma or bias. Dundon notes they don’t ask students or families to necessarily disclose if they’re facing food insecurity for that reason.
However, FWCS’s data indicates that 70 percent of Fort Wayne Community Schools’ students are under the free and reduced umbrella.
Dundon notes these classes are often the first time students are exposed to certain cooking-related concepts. In other words, these youth are often blank canvases and eager to learn. The skills acquired in the classes can improve quality of life both in the short and long term.
“(They started by) learning how to cut properly and use measuring cups and spoons,” she says. “With measuring, they learned how to read conversions and how to do (them). And then the next four days, they spent the class periods making different recipes, so they made pumpkin pancakes, a salad and healthy smoothies, for example.”
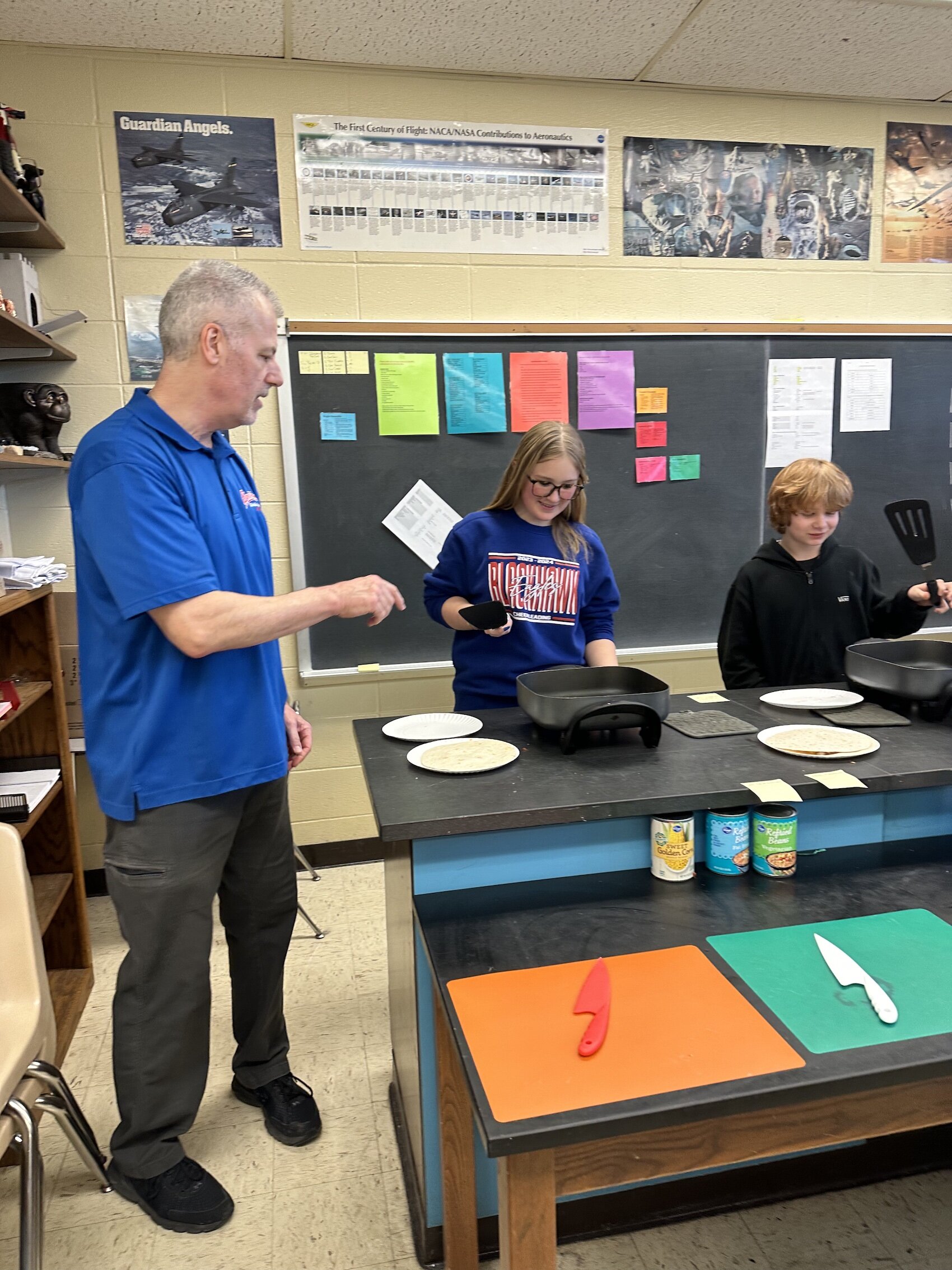
Dundon says this program also exposes students to new foods and kitchen safety, like how to safely use a knife. For some, the outcomes might be more delayed. For example, she’s hopeful that this experience can plant a seed that grows into something more substantial later in life.
“We’re watching those kids as they grow and (seeing) what kind of choices they make,” she says. “(For example), did they make a choice to go into something culinary? We have culinary programs (at FWCS) that give them hands-on experiences (that might inspire them) to want to be a chef, go into culinary arts or (become) a nutritionist or a dietitian, so as kids go through the system, we definitely want to monitor and see what they choose to do.”
Speaking of monitoring, Dundon says they conduct a pre and post-assessment to see how students’ knowledge and skill sets have grown as a result of this form of experiential learning.
“We showed the students four different photos and asked them which one was holding a knife correctly,” she says. “From the pre-test to the post-test, the students had a growth of 53 percent.
When asked how many servings of fruit and vegetables should we aim for every day, the students had an increase in knowledge of 46 percent.”
Waldron says while these results are encouraging, solving complex and layered problems like food insecurity and obesity will require more than a few years to see meaningful change on a community level.
“We all have to be very mindful that it’s probably going to be at least 10 years until we start seeing actual changes in outcomes, such as obesity or food insecurity,” she says. “As a state that took a long time to get where it got, it’ll take a long time to begin to see betterment in that.”
Despite being optimistic, she wants to manage expectations around potential outcomes and maintain close working relationships with the grantees. For example, that means learning about what’s working and where there might be room for fine-tuning.
In the longer term, Waldron says she hopes to facilitate coalitions and create an environment that’s supportive and collaborative. The hope is that community agencies would share challenges and opportunities with the local health department and each other. After all, in her estimation, the nonprofits and other community-based entities are the ones doing the work day in and day out. They’re the authority on solutions.
“We have some very robust community-based organizations doing great work,” she says. “We want to hear from them. What do you think the biggest gaps are that the public health (department) should be stepping in to (address)? So we’re in this full year or two of discerning before we say we know more than they do. Because they’re the experts currently in these areas, and we’re learning from them every day.”
The creation of this article is in part thanks to a collaborative effort to provide more local coverage of public health matters through support from the Knight Foundation.













